Acute Cardiac Care Unit, Crosshouse Hospital, NHS Ayrshire & Arran, Scotland
Within cardiology, there is a cohort of patients who require prolonged IV access, such as those with decompensated heart failure and those with infective endocarditis. Moreover, there is also a group of patients who have difficult IV access (DIVA). It was identified around 5 years ago that midline may plug a gap in care provision for these groups of patients. These devices can also provide an alternative to patients having multiple cannulas placed or being referred for PICC, which was often not the correct ‘line’ for patients, even though it was the only option we had.
For those with DIVA, this often resulted in patients experiencing not only delays to therapy, but potentially length of hospital stays. It was envisaged that a midline service would improve patient satisfaction with a reduction in cannulation/venepuncture attempts.
Like other service provision and developments, COVID put a marked delay on the implementation of this project and development of this service.
I currently work as a Senior Advanced Nurse Practitioner (ANP) within a cardiology in-patient area with cardiology day unit commitment. The following is an account on how this service was implemented and developed in my workplace.
-
First steps of midline introduction inside our unit
There was an enthusiastic buy in from the wider team of nurses, ANPs, consultant cardiologists and industry on the potential benefits midlines could offer patients within our organisation.
Within our unit, the enthusiasm was infectious. However, it was not just a matter of proceeding without further consideration. Unlike our medical colleagues who have traditionally acquired the skill of seeing, doing, then teaching, from a nursing perspective, the governance required to acquire these new skills to ensure both nurses and patients receive safe and quality care.
-
Governance and support from the manufacturers
Whilst governance was being addressed, which I knew could take some time, we were provided ultrasound placement and supervised manikin practice with the assistance of manufacturers, education resources and modules around placing lines.
The progression of this service happened thanks to a wider buy in from a working group of ANP’s, a very supportive consultant anaesthetist (who provided direction and acted as mentor/supervisor), industry personnel and a ward nursing team. This was instrumental in progressing this service. The governance process was secured to allow nurses to place midlines independently and safely.
-
Internal organisation of a nurse led midline service
Alongside governance, paperwork on the care and maintenance of midlines were developed. An ‘insertion bundle sticker’ that could be placed in the medical notes was introduced.
 Picture 1: Bundle sticker (Credits: Ali Meikle – Consultant Anaesthetist)
Picture 1: Bundle sticker (Credits: Ali Meikle – Consultant Anaesthetist)
One of the biggest challenges to providing a nurse led midline service was gaining supervised practice. This was very much reliant on myself having dedicated time to place the midline, coordinating, and having access to my consultant anaesthetist (expert placing midlines) supervisor with his own clinical commitments, having nursing staff free to assist and lastly, having suitable patients for a midline placement.
Initially, it was identified between myself and my mentor to have ten supervised placements as sign-off as a minimum. In reality, it took around fourteen attempts in total before I placed lines confidently and independently. It took three months from March 2022 to June 2022 for me to achieve my sign-off. On a personal level, each attempt, whether initially successful or not, was a learning opportunity to be had. When a line was straight forward and was an easy pass, it felt immensely satisfying. In parallel, when there was a challenging patient or failure, it led to frustration and a knock to confidence. As I now supervise others, this is something that I tell them to expect and appreciate for themselves.
After each placement, I had a better understanding of the importance of having the right layout of environment for placing a midline, patient placement, positioning and equipment. During this test of change in practice, we secured a trolley specifically for midline placement, which could be taken to patient chair or bedside.
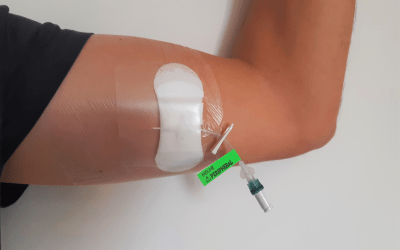
 Picture 2: Specific midline placement trolley
Picture 2: Specific midline placement trolley
-
Nurses training
Once I had gained sign off and with the enthusiasm of the nursing staff, I secured designated time within my job plan (initially for one hour, twice per week) so that suitable patients could be allocated to these slots. This designated time allowed us not only to gain more time to place lines, but to also equip fellow nurses time to see lines being placed. It also gave them time to place lines themselves with supervision once I was signed off as independent.
As stated earlier, I work in a cardiology ward with a co-attached cardiology day unit. Staff were already competent in the care and maintenance of patients with PICC lines and in our high care environment, those with central lines. Education for the ward staff was provided on the use, care and maintenance of midlines.
The daily safety huddle on the ward now comprises of asking if there is anyone suitable for midlines (those likely needing IV access for five days or more or those with difficult IV access, defined as those with x2 failed attempts at cannulation). It also includes any problems with those who have had a midline in place. On top of the designated slots available, if capacity allowed, we would attempt to place further lines/urgent cases such as those with DIVA.
As I was now signed off as competent to place lines independently, I developed a structured program to train others. After nursing staff had completed the industry modules and had observed midlines being placed, they could begin their supervised practice.
To make it possible for another nurse to help with supervision of future nurses, I attempted to concentrate on getting sign off for her instead of having a lot of nurses in training at the one time. This ensured when I was not on duty and there was a midline required that there would be available personnel to do this. An oversight from me was as a Non-Medical Prescriber (NMP). There was a requirement to ensure there was a Patient Group Direction (PGD) for subcutaneous lignocaine (local anaesthetic) to be administered by nursing staff who doesn’t hold a NMP qualification. This was devised and passed through the PGD Prescribing Team. By having this PGD in place, their independent practice was promoted and it allowed them to place midlines truly independently.
-
Results
Through a small study of patients there has been over 120 midlines placed to date in just over one year. We now have a pool of three nurses who practice independently in placing midlines and we have a further two nurses due to complete their independent practice in the next two months.
Data has been collected on every patient. Part of this involves patients having a questionnaire to complete. They are overwhelmingly satisfied with the service. 100% of midlines in last year have been placed within one day or less from referral for line to line being placed. Patients’ comments include “better, more comfortable”, “much better than multiple cannulas” and “Why has this not been offered before?”.
Furthermore, there has been no SABs and the dwell times of midlines have increased with further education for example with daily walk rounds to speak to nurses and the development of an education board. There has been lots of interest from other areas of my hospital and now that we are in a position of having more nurses trained and able to supervise others, there is a plan to spread the same project to other areas. Additionally, our PICC line referral rate has also fallen by 55% in the last year.
Conclusion
There is no doubt that the introduction of a midline service has been a success. The process from idea to the full implementation of the service took around 5 years (COVID years). However, despite these challenges, we have clearly identified that suitably trained nurses can place the “right line at the right time”.
Thank you to Dr A Meikle (Consultant Anaesthetist) for acting as clinical mentor, Vygon UK and the fantastic and enthusiastic nursing staff of the Cardiology Day Unit, Crosshouse Hospital.




0 Comments