Practice and Use of Digital Sedation
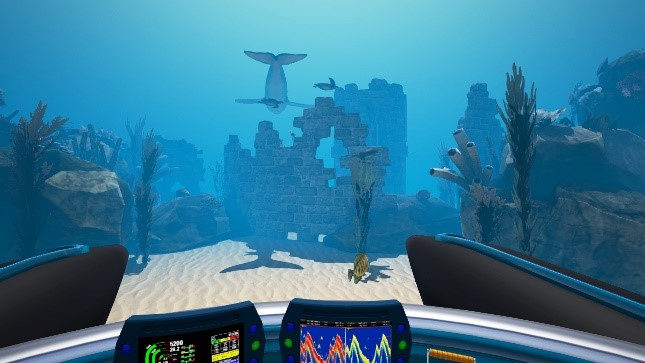
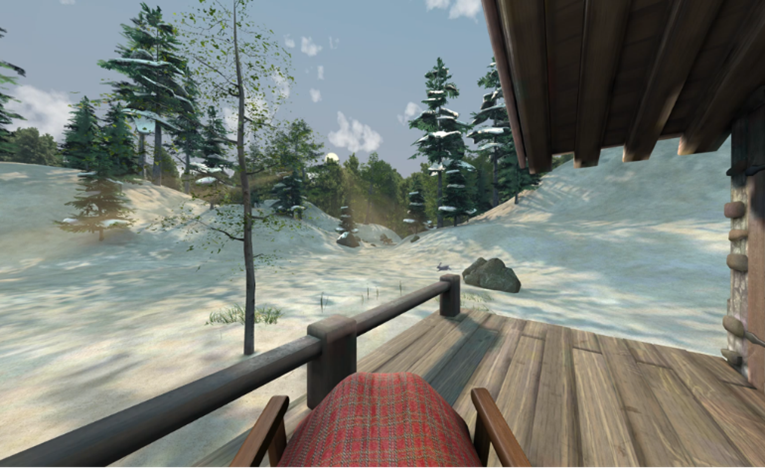
In the waiting room of a surgical service or a vascular access unit, patients can benefit from a new device to help them relax before the surgical procedure. The medical team can give them the option of wearing a virtual reality headset and to go on a trip. They can go scuba diving in the bottom of the oceans with a whale or enjoy a pleasant walk in the woods, far from bad weather. The Digital Sedation™ is based on stylized images, yet realistic. They are in 3D and in 360°. The relaxing music, the breathing exercises and the narration help them distress. The very immersive nature of this high-tech material allows an adhesion of the patient that is almost constant. It is intuitive and easy to use. It is more than a simple relaxation or distraction since it has the effects of self-hypnosis with a period of induction, maintenance, anchoring and awakening. The time and duration of the application can change depending on the needs.

For the past few years, the use of virtual reality has been increasing in the world of health, neurology, re-education, psychiatry, treatment of neurosis, phobias and now, in the interventional radiology suites and operating rooms. Virtual reality is quite different from augmented reality: In virtual reality, the patient is inside a virtual environment whereas in augmented reality, the objects become visible on beside real elements.
Digital Sedation Bibliography
However, there is still a lack in bibliography about it. 3 major journals are available1,2,3 and confirm the efficiency of the techniques of virtual reality. They confirm the importance of the quality of the devices: the headphones, the mask, and the software. The experimental studies are mainly based on healthy volunteers but its effectiveness is represented in imaging during functional MRI4 . On the clinical aspect, the efficiency of virtual reality is now recognized. Its use is recommended when it comes to burn dressings5. Its use is also expanding to surgery units: in urology6, orthopedy7, breast surgery8, and vascular access9,10,11.
In our own experience, we have been testing since 2014 this device in the preoperative period, and almost all the subjects have stated that their anxiety diminished by more than 50%, based on the evaluation scale that was proposed to them.
Digital Sedation Use
These devices are now alternatives to premedication or sedative and anti-anxiety drugs. Moreover, they can replace clinical hypnosis that is time consuming and that can’t always be proposed to patients, considering the time it takes or the lack of availability, despite the rising number of trained healthcare professionals.
The Digital Sedation™ is an alternative therapeutic solution that can be adapted to various clinical situations by adapting to the patient’s age (from 6 years), duration and type of intervention.
This technology is also of interest and valuable during chemotherapy to manage patient anxiety and provides a better patient experience of his care pathway.
Healthcare workers’ role
In practice, healthcare workers have an essential role in the reception of patients during this experience, that is sometimes the first one that they would go through. The commitment of the healthcare workers and the affirmation of their availability during the act are success guarantees. The headset is placed on the patient’s head a few minutes before the act to let some time for the hypnotic induction. Contact is kept during the act. The operator or the assistant caregiver can for instance let the patient know in a calm tone when it is time for local anaesthesia, venepuncture, or the creation of the subcutaneous pocket of a port. A time distortion is often noticed: patients assess an intervention time shorter than reality.
Calmness that can easily be acquired by patients can also spread to the care teams.

Conclusion
Self-hypnosis or Digital Sedation™ through virtual reality in health care facilities is no longer virtual and not yet well established, but real and effective. It must be integrated in the care units and in the patients’ care process.


Bibliography
- Gupta A, Scott K, Dukewich M; Innovative Technology Using Virtual Reality in the Treatment of Pain: Does It Reduce Pain via Distraction, or Is There More to It? Pain Medicine 2017; 0: 1–9 doi: 10.1093/pm/pnx109.
2. The effectiveness of virtual reality distraction for pain reduction: A systematic review Malloy K, Milling L Clinical Psychology Review 30 (2010) 1011–1018.
3. The Use of Virtual Reality and Audiovisual Eyeglass Systems as Adjunct Analgesic Techniques: A Review of the Literature Wismeijer A, Vingerhoets J. Ann Behav Med 2005, 30(3):268–278
4. The Analgesic Effects of Opioids and Immersive Virtual Reality Distraction: Evidence from Subjective and Functional Brain Imaging Assessments; Hoffman H, Richards T,Van Oostrom T, Coda A, Jensen M, Blough D, Sharar S. Anesth Analg 2007;105:1776 –83.
5. SURGERY – PROCEDURES, COMPLICATIONS, AND RESULTS. BURNS PREVENTION, CAUSES AND TREATMENT; MCLAUGHLIN E, PATERSON A. Nova Science Publishers, Inc. New York.
6. Virtual Reality Distraction during Endoscopic Urologic Surgery under Spinal Anesthesia: A Randomized Controlled Trial Moon J, Shin J, Chung J, Ji SW, Kim W J. Clin. Med. 2019, 8, 2; doi:10.3390/jcm8010002
7. Virtual Reality as an Adjunctive Nonpharmacological Sedative During Orthopedic Surgery Under Regional Anesthesia: A Pilot and Feasibility Study; Chan P, Scharf S, Anesth Analg 2017.
8. M. Berlière, S. Lamerant, P. Piette et al, « Potentiel benefits of hypnosis sedation on different modalities of breast cancer treatment, » Cancer Research, vol. 75, no. 9, pp. suppl, 2015.
9. Is Virtual Reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of pediatric Virtual Reality for Acute Procedural Pain Management; Gold J, Mahrer N Journal of Pediatric Psychology, 2017, 1–10 doi: 10.1093/jpepsy/jsx129.
10. Rosay H, Laurent C, Delhomme I, Hamon G, Thiot A, Dupre A; Autohypnosis and Virtual Reality decrease preoperative anxiety ASA 2017
11. Effects of passive music therapy on anxiety and vital signs in lung cancer patients undergoing peripherally inserted central catheter placement procedure Qianqian Mou, Huiqiong Xu The journal of vascular access Vol 21, Issue 6, Nov 2020 . doi.org/10.1177/1129729820908088
12. SFAR (Société Française d’anesthésie et de réanimation), E-sfar 2019 – Réalité virtuelle et hyponose : anesthésie 3.0 ?, Fev 2020, https://www.youtube.com/watch?v=fRVoMSii68A





0 Comments